This background video contains only decorative imagery and does not convey meaningful information.
Featured Article
The Lipid Membrane: The Unsung Hero of Cellular Health
The cell membrane, a lipid bilayer just a few nanometers thick, plays a critical role in cellular function by regulating nutrient transport, immune signaling, and maintaining overall cell integrity. Essential fatty acids, like omega-3 and omega-6, are crucial for maintaining membrane fluidity and functionality, which supports energy production, cellular communication, and resistance to degenerative disease.
-
Dr. Bruce Hoffman | 01.13.2026
A Roadmap for Hypersensitive MCAS Patients and BodyBio PC
One of the most common questions I get is this:“I’m so reactive. Should I even be taking BodyBio PC? Every time I try, I feel worse.”Let’s clear th... -
Ashley Palmer | 01.05.2026
The Missing Link in Longevity: Repair the Cell First, Everything Else Follows
You've cleaned up your diet. You're taking the supplements everyone's raving about. Maybe you've even invested in a longevity protocol complete wit... -
Ashley Palmer | 12.17.2025
Fat Facts: Understanding Omega-3 & Omega-6 for Better Healt
Essential fatty acids are among the most influential nutrients in human biology — yet they’re also some of the most misunderstood. Omega-3s tend to... -
Ashley Palmer | 12.17.2025
Resolution vs. Suppression: How SPMs Support the Body's Natural Inflammation Response
You take ibuprofen for your knee. Four hours later, the pain's back.This happens because suppressing inflammation and resolving inflammation are tw... -
Ashley Palmer | 12.09.2025
What are Systemic Enzymes and Do You Need Them for Optimal Health?
You've probably heard about digestive enzymes, which help break down food. But there's another type of enzyme that works completely differently, an... -
Ashley Palmer | 12.03.2025
Cold Plunging and Women’s Health: What to Know Before You Try It
You've seen the videos: influencers stepping out of ice baths looking energized, refreshed, ready to conquer their day. Cold plunges are everywhere... -
Ashley Palmer | 11.25.2025
How Sugar and Stress Impact Gut Health (and How to Support It During the Holidays)
Between the office party appetizers, your aunt's famous cookies, and that second or third glass of wine at dinner, your gut is working overtime thi... -
Ashley Palmer | 11.25.2025
The Science of Cellular Stress — and How to Protect Yourself From It
Stress doesn't just live in your head. It lives in your cells.Most people understand stress as something psychological — deadlines, relationships, ... -
Jess Kane | 11.07.2025
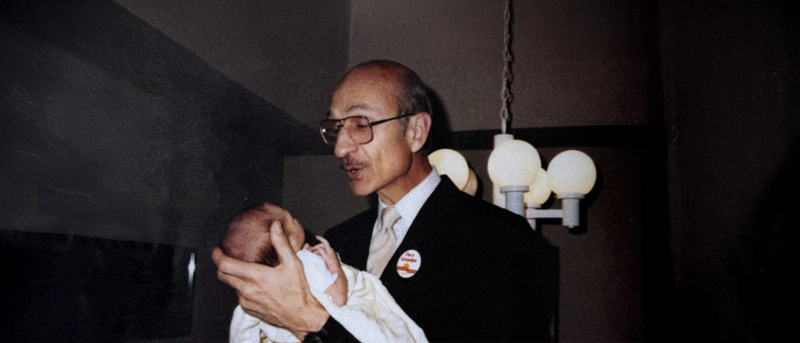
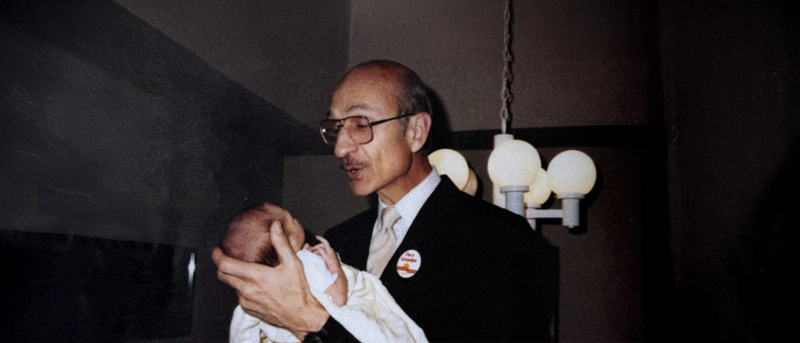
The History of BodyBio: Pioneering Cellular Health Since 1998
When you see a new wellness brand pop up, it often looks shiny, polished, and backed by a well-oiled marketing machine. But BodyBio isn’t that stor...








